Patient's Right to Consent to Medical Procedures from the Perspective of Health Law, Bioethics, and Human Rights
DOI:
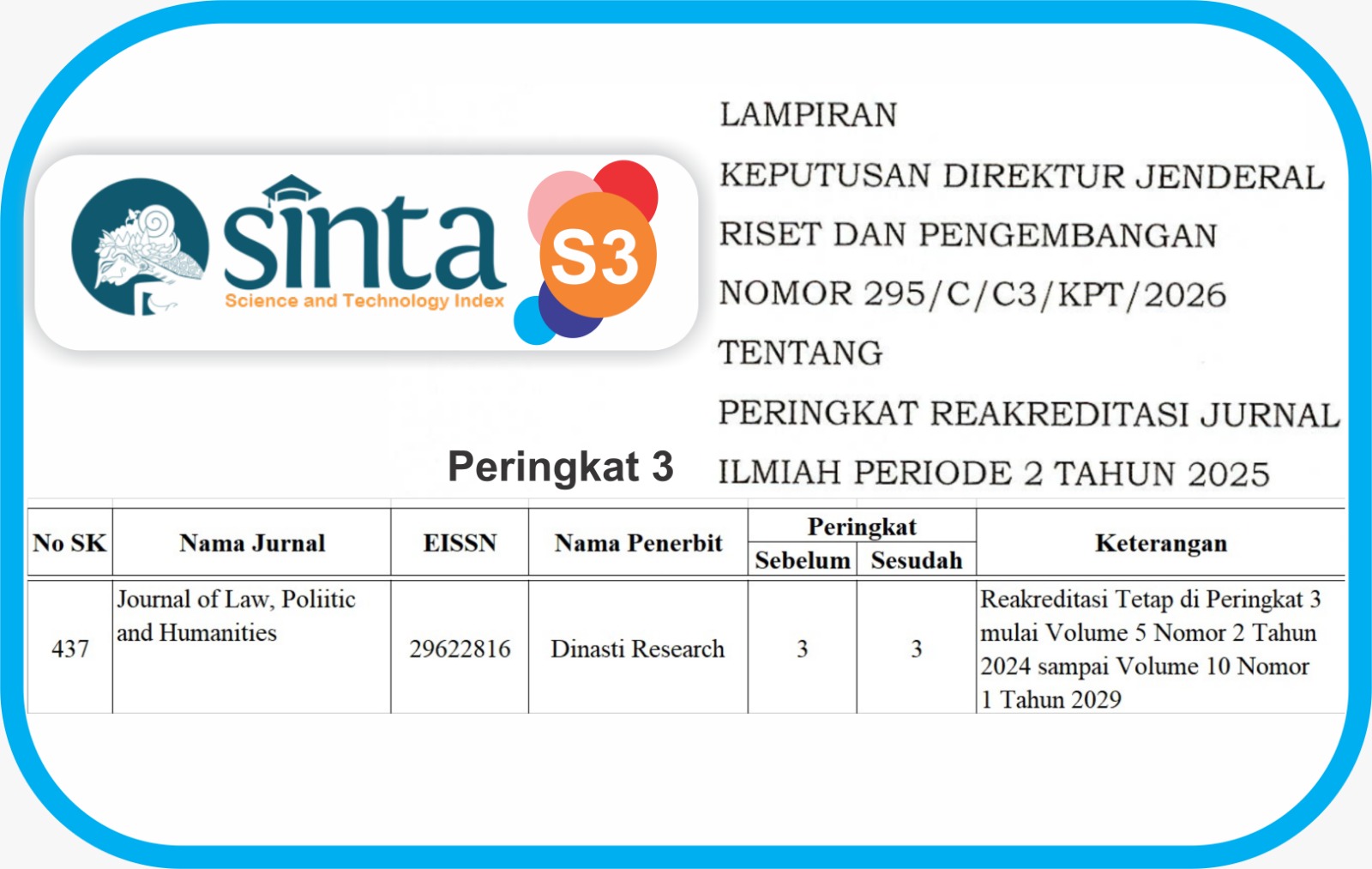
https://doi.org/10.38035/jlph.v5i4.1505Keywords:
Patient's Rights, Medical Consent, Health Law, Bioethics, Human RightsAbstract
The patient's right to consent to medical procedures is a vital element in the relationship between patients and healthcare providers, connected to health law, bioethics, and human rights, all focusing on the protection of patient autonomy. This study analyzes the patient's right to consent from the perspectives of health law, bioethics, and human rights, and identifies challenges in its implementation in Indonesia. A normative method is employed with legislative, conceptual, and comparative approaches. Data is gathered by analyzing national regulations, bioethical principles, and literature on human rights. Descriptive-analytical analysis was used to explore the synergy between these three perspectives in medical consent implementation. Findings reveal that the patient's right to consent is regulated by Law No. 17 of 2023 and other relevant regulations. Bioethics stresses respecting patient autonomy, while human rights ensure access to information and the freedom to consent. Challenges include paternalistic cultural attitudes, low public awareness, and inadequate healthcare facilities. Recommendations include strengthening regulations, providing bioethics training for healthcare professionals, and educating the public to safeguard patient rights in medical procedures in accordance with health law, bioethics, and human rights.
References
Anggraini, D. (2020). Hak Pasien dalam Perspektif Hukum Kesehatan di Indonesia. Jakarta: Rajawali Press.
Beauchamp, T. L., & Childress, J. F. (2013). Principles of Biomedical Ethics. Oxford University Press.
Callahan, D. (2003). Principlism and communitarianism. Journal of Medical Ethics, 29(5), 287–291.
Elmadiani, R. A. (2020). Penerapan prinsip bioetika dalam persetujuan tindakan kedokteran. Repository UGM.
Gillon, R. (1994). Medical ethics: Four principles plus attention to scope. BMJ, 309(6948), 184–188.
Gostin, L. O., & Gruskin, S. (2004). Human rights approach to public health policy. Journal of Public Health Policy.
Inspektorat Jenderal Kementerian Kesehatan. (2021). Pentingnya sistem pengawasan dalam implementasi kebijakan pelayanan kesehatan. Kemhan.
Jonsen, A. R., Siegler, M., & Winslade, W. J. (2015). Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. McGraw Hill Professional.
Kementerian Kesehatan Republik Indonesia. (2008). Peraturan Menteri Kesehatan Nomor 290/MENKES/PER/III/2008 tentang Persetujuan Tindakan Kedokteran. Jakarta: Kementerian Kesehatan RI.
Marzuki, A. (2020). Kesenjangan pelaksanaan informed consent di Indonesia: Tinjauan empiris dan hukum. Jurnal Hukum Kesehatan Indonesia, 12(3), 245-258.
Mulyani, T. (2020). Tanggung gugat dokter atas operasi tanpa persetujuan pasien. Repository Ubaya.
Nasution, B. J. (2023). Informed consent pada kasus kegawatdaruratan di rumah sakit. Review Unnes.
Nugroho, T. (2018). Hak asasi pasien dalam perspektif hukum dan etika kedokteran. Jurnal Etika Kedokteran, 10(1), 15-29.
Pawestri, A. (2017). Hak penyandang disabilitas dalam perspektif HAM internasional dan HAM nasional. Jurnal Hukum, 2(1).
Presiden RI. (2023). Undang-Undang Republik Indonesia Nomor 17 Tahun 2023 tentang Kesehatan. Undang-Undang, 187315, 1–300.
Pratiwi, A. A. (2019). Pengaruh edukasi terhadap pengetahuan tentang hak dan kewajiban pasien. Jurnal Ilmiah Kesehatan Promotif, 6(1), 45-50.
Pusat Bioetik Nasional. (2019). Prinsip Bioetika dalam Praktik Medis di Indonesia. Jakarta: Penerbit Bioetik Nusantara.
Purba, G. P. (2024). Tanggung jawab dokter terhadap pasien ditinjau dari aspek hukum. Majelis, 1(3).
Rahman, A. (2021). Tantangan implementasi informed consent di fasilitas kesehatan daerah terpencil. Jurnal Hukum Kesehatan Indonesia, 9(2), 45-58.
Smith, B. T., Warren, C. M., Rosella, L. C., & Smith, M. J. (2023). Bridging ethics and epidemiology: Modelling ethical standards of health equity. SSM – Population Health, 24. https://doi.org/10.1016/j.ssmph.2023.101481
Suharyo, D., Santoso, B., & Wulandari, R. (2019). Analisis pemahaman pasien terhadap hak atas persetujuan medis di rumah sakit daerah. Jurnal Etika Kedokteran Indonesia, 7(1), 20-32.
UNESCO. (2005). Universal Declaration on Bioethics and Human Rights.
United Nations. (1948). Universal Declaration of Human Rights.
United Nations. (1966). International Covenant on Economic, Social and Cultural Rights (ICESCR).
Undang-Undang Nomor 29 Tahun 2004 tentang Praktik Kedokteran.
WHO. (2018). Patient Safety: Global Action on Patient Safety. Geneva: World Health Organization.
WHO. (2020). Universal Health Coverage: Moving Towards Better Health for All. Geneva: World Health Organization.
World Health Organization. (2021). Informed Consent: Ethical and Legal Perspectives. Geneva: WHO Press.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Ni Putu Parvathi Priyadarshini, I Gusti Ayu Putri Kartika

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish their manuscripts in this journal agree to the following conditions:
- The copyright on each article belongs to the author(s).
- The author acknowledges that the Journal of Law, Poliitic and Humanities (JLPH) has the right to be the first to publish with a Creative Commons Attribution 4.0 International license (Attribution 4.0 International (CC BY 4.0).
- Authors can submit articles separately, arrange for the non-exclusive distribution of manuscripts that have been published in this journal into other versions (e.g., sent to the author's institutional repository, publication into books, etc.), by acknowledging that the manuscript has been published for the first time in the Journal of Law, Poliitic and Humanities (JLPH).